Abstract
Background: Pre-eclampsia is a hypertensive disorder of pregnancy that affects about 5% of all pregnancies; however, its pathogenesis remains poorly understood. About 1% of pre-eclampsia cases will progress to a severe form termed HELLP syndrome characterized by Hemolysis, Elevated Liver enzymes, and Low Platelet counts. We have previously shown that abnormal activation of complement is a driver of disease in a subset of patients with HELLP syndrome (Vaught et al. 2016 and 2018). Based on these studies, we proposed that germline variants in complement regulatory genes predispose to HELLP in the setting of pregnancy, a complement amplifying event. However, whether complement dysregulation correlates to disease severity in HELLP syndrome is unclear. In addition, the contribution of complement activation to the onset or severity of pre-eclampsia remains unknown. We hypothesized that patients with pre-eclampsia harboring complement gene variants are at increased risk for progression to HELLP syndrome and worse maternal and fetal outcomes due to dysregulation of the complement system.
Methods: In this prospective cohort study, patients with the pregnancy-associated hypertensive disorders including HELLP or pre-eclampsia were enrolled after diagnostic validation with the Tennessee and ACOG classification criteria, respectively. In total, 24 women with HELLP and 42 women with pre-eclampsia were enrolled and followed through their hospital course and compared with 47 healthy normotensive pregnant women. Both maternal and fetal clinical outcomes were recorded. Delivery before estimated gestational age < 23 weeks was considered previable, and intra-uterine fetal death (IUFD) was characterized as death of the fetus in utero during the pregnancy. Targeted sequencing of 13 genes known to regulate the alternative complement pathway was performed, and non-synonymous, heterozygous germline variants with a minor allele frequency less than 0.01 were identified. A functional assay for complement activation, the modified Ham assay (mHam), was performed in a subset of cases with available serum samples. The mHam is based on the principle that a cell line lacking surface complement regulators is susceptible to complement mediated cell death; non-viable cells > 20.5% is considered a positive test.
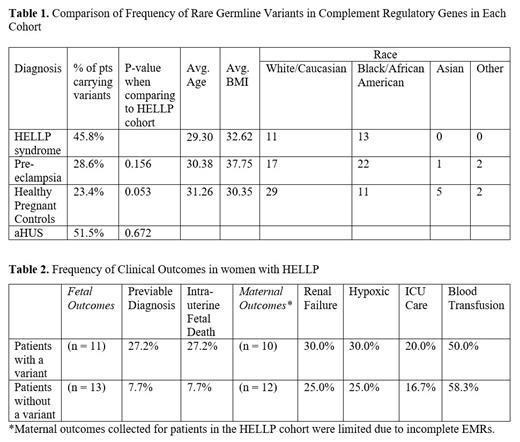
Results: The frequency of rare germline variants in the HELLP cohort was 45.8%, comparable to a well-established complement mediated disease (aHUS, Table 1). By comparison, the frequency of germline variants in the pre-eclampsia and control cohort was 28.6% and 23.4%, respectively. Of the 14 patients with sera available to perform the mHam, 57% of HELLP syndrome patients had a positive mHam as compared to 0% of the controls (p = incalculable). Among patients with HELLP syndrome, those with a complement gene variant were more likely to have a poor clinical outcome compared to those without a variant. Specifically, 3/11 patients with variants versus 1/13 patients without variants were diagnosed at a previable stage and/or experienced IUFD (p = 0.19). There was no difference in the rate of HELLP onset after 28 and 34 weeks between the two groups. Notably, when comparing the cohort of HELLP patients harboring variants to the cohort without, patients with variants had higher rates of acute renal failure, hypoxia, and ICU care, but a lower frequency of blood transfusions (Table 2).
Conclusion: Patients with HELLP syndrome harbor rare germline variants in complement genes at a greater frequency than controls (p = 0.05) and a similar frequency to aHUS, a known complement mediated disease. HELLP syndrome patients also carry mutations at a higher frequency than women with pre-eclampsia (p = 0.16) who have a similar rate of variants as controls. This suggests that complement gene variants predispose to progression of pre-eclampsia to HELLP syndrome where the gene variant and pregnancy provide a first and second 'hit' similar to other complement disorders. Patients with rare complement-associated variants are also more likely more susceptible to severe disease manifestations.
Chaturvedi: UCB: Other: Advisory board participation; Sanofi Genzyme: Other: Advisory board member; Alexion: Other: Advisory board member; Dova: Other: Advisory board member; Argenx: Other: Advisory board member.